Abstract
Introduction:
Vaso-occlusive crisis (VOC) is a leading cause of morbidity in children with sickle cell disease (SCD) and is the most common reason for hospitalization. Frequent and prolonged hospitalization is a risk factor for development of acute chest syndrome and increased mortality, and also leads to decreases in school attendance and quality of life measures. Furthermore, inpatient care accounts for a large proportion of total disease-related costs.
A sickle cell day hospital (DH) is an outpatient facility with several beds, staffed by hematology/oncology trained attending physicians, fellows, nurse practitioners and bedside nurses, all with expertise in caring for patients with SCD. The concept of the DH as an alternative to the emergency department (ED) for treatment of VOC has been explored in adults, with evidence for reduced hospitalization rate, superior pain relief and significant cost-savings. In pediatrics, there is limited data on the utility of a DH for VOC management.
We hypothesize that pediatric patients with SCD presenting to our institution with acute VOC who are managed in the DH will have a lower rate of inpatient admission than those managed in the ED.
Methods:
We performed a retrospective chart review of children aged 4 to 21 years with HbSS, HbSC, HbSβ0- or β+- thalassemia who received initial treatment for uncomplicated VOC with IV opioids in the DH or ED at the Children's Hospital at Montefiore during three consecutive calendar years. Patients were excluded if they had any of the following at the time of presentation: pain score < 7, temperature > 38.0°C, decrease in oxygen saturation >2% below baseline or <92% on room air, new chest x-ray infiltrate, headache or other neurological symptoms, or evidence of splenic sequestration. Patients selected for the ED cohort were limited to those who presented during the hours when the DH was open. Additionally, patients transferred from the DH to the ED or vice versa at any time during the visit were excluded. We abstracted data from the charts of 60 unique patients for each site to allow for assessment of our primary outcome of need for inpatient admission at the time of initial visit, as well as secondary outcomes including time to initial and rescue doses of opioid analgesic. The study was approved by the Institutional Review Board at Montefiore Medical Center.
Results:
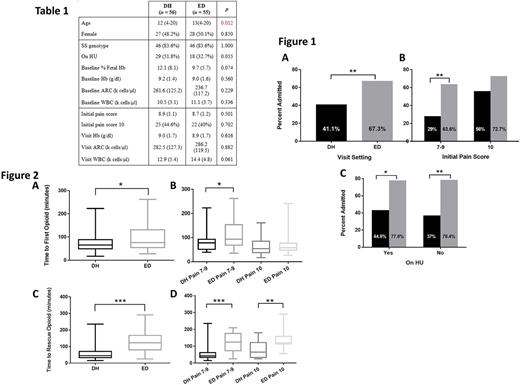
Data from 56 DH and 55 ED patients have been analyzed to date. In general, the cohorts had similar demographics, sickle cell disease status, and pain scores (Table 1), except for younger age in the DH cohort (median 12 years vs 13 years, p = 0.012). Patients who presented to the DH were significantly less likely to be admitted than patients who presented to the ED, with admission rates of 41.1% and 67.3%, respectively (p= 0.008) (Fig 1A). Admitted patients from each setting were further stratified by pain score at presentation (Fig 1B) and by hydroxyurea (HU) status as a surrogate marker of disease severity (Fig 1C). In patients with an initial pain score of 10, there was no significant difference in admission rate based on treatment location (DH 56% vs ED 72.7%, p= 0.362). In contrast, patients with an initial pain score of 7-9 were significantly less likely to be admitted from the DH than from the ED (29% vs 63.6%, p= 0.007). DH-managed patients were significantly less likely to be admitted regardless of HU status compared to ED-managed patients (on HU: 44.8% vs 77.8%, p= 0.036; not on HU: 37% vs 78.4%, p= 0.002).
Secondary analyses showed a significant difference between the DH and ED in the median time to initial (Fig 2A) and rescue (Fig 2C) opioid doses (initial: 65 mins vs 76 mins, p= 0.044; rescue: 45 mins vs 123 mins, p < 0.001). This comparison was further stratified based on pain score at presentation, and demonstrated significantly longer median time to initial dose of opioid in the ED for those patients with initial pain score of 7-9 (78 mins vs 93 mins, p= 0.032 - Fig 2B), but no significant difference for those with initial pain score of 10. Time to rescue dose of opioid was significantly longer for patients seen in the ED, regardless of pain score (pain 7-9: median 43 mins vs 125 mins, p < 0.001; pain 10: median 65 mins vs 120 mins p= 0.006 - Fig 2D).
Conclusions:
A dedicated pediatric sickle cell day hospital is an effective setting for the management of uncomplicated acute VOC. Treatment in this setting is associated with decreased rates of inpatient admission and faster administration of appropriate analgesics.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal